Syllabus Edition
First teaching 2025
First exams 2027
Diversity in Sex Development (AQA A Level Psychology): Revision Note
Exam code: 7182
Androgen insensitivity syndrome
Diversity or differences in sex development (DSD) is the modern term for the congenital variations in chromosomal, hormonal or anatomical sex characteristics that mean a person’s sexual development differs from the typical XX or XY pattern
The term DSD replaces older labels such as “disorders of sex development", "intersex", or "atypical sex chromosome patterns"
Androgen insensitivity syndrome (AIS) impacts the development of a person’s genitals and reproductive organs and affects approximately 1 in 20,000 individuals
People with AIS have XY (male pattern) chromosomes
The cause of AIS is genetic, involving the inability to respond to androgens fully or partially due to androgen receptor dysfunction, i.e., insensitivity to androgens that produce a physical male appearance
A consequence of this is that it impacts the sex development of typical male genitals
E.g., a penis does not form or is underdeveloped, meaning that the child's genitals may develop as female or are underdeveloped as male
There are two types of AIS:
Complete androgen insensitivity syndrome (CAIS), where the genitals of a person with CAIS appear female
CAIS can be difficult to spot at birth, as the genitals usually look like those of a biological female; it is usually diagnosed at puberty when menstruation does not start and other secondary sexual characteristics do not develop, such as pubic and underarm hair
Partial androgen insensitivity syndrome (PAIS), where the genitals of a person with PAIS may appear as female or male
PAIS is usually discovered at birth because a baby's genitals are not as expected for a baby boy or baby girl
The genetic alteration that causes AIS is passed along the female line to the child
Women who carry the genetic alteration will not have AIS themselves, but as their genes are passed on to the embryo during fertilisation, there's a 1 in 4 chance that each child they have will be born with AIS
In terms of reproductive organs, a person with AIS has no uterus or ovaries, as their genotype is male, XY
Klinefelter's syndrome
Any combination of sex chromosomes other than XX (female) and XY (male) is referred to as atypical
These patterns can be inherited or may occur at conception or be due to division of the human reproductive cells before fertilisation of the egg and sperm cells
All babies will have an X chromosome, as human life cannot exist without this, but XXY, XYY, and XO (where the additional X is missing) are all possible
Klinefelter’s syndrome (KS)
KS affects about 1 in every 600 males (Klinefelter’s Syndrome Association, 2023) and involves having an extra X (female) chromosome, giving the atypical sex chromosome pattern of XXY and an excess of oestrogen in the body
KS is due to an error in the egg cell when it develops or if the father’s sperm carries an extra X chromosome
KS may not be discovered until puberty, especially in the case of the much more common and milder ‘mosaic’ KS, where only some of the boy’s cells have the XXY chromosomal pattern and the others are normal
KS is incurable, but treatment with additional testosterone can increase muscle and bone development, though it cannot reverse infertility
The characteristics of Klinefelter’s Syndrome
Physical | Cognitive |
|---|---|
Small testes, producing low levels of testosterone, and small penis | Poor language skills that affect reading and writing abilities |
No facial hair and limited pubic and body hair | Poor mathematical skills |
Broader hips, long legs and arms compared to the torso and the development of breast tissue | Quiet, shy temperament with attention difficulties |
Delayed or incomplete puberty (some boys do not go through puberty at all) and infertility is likely | Increased risk of anxiety disorders and/or depression |

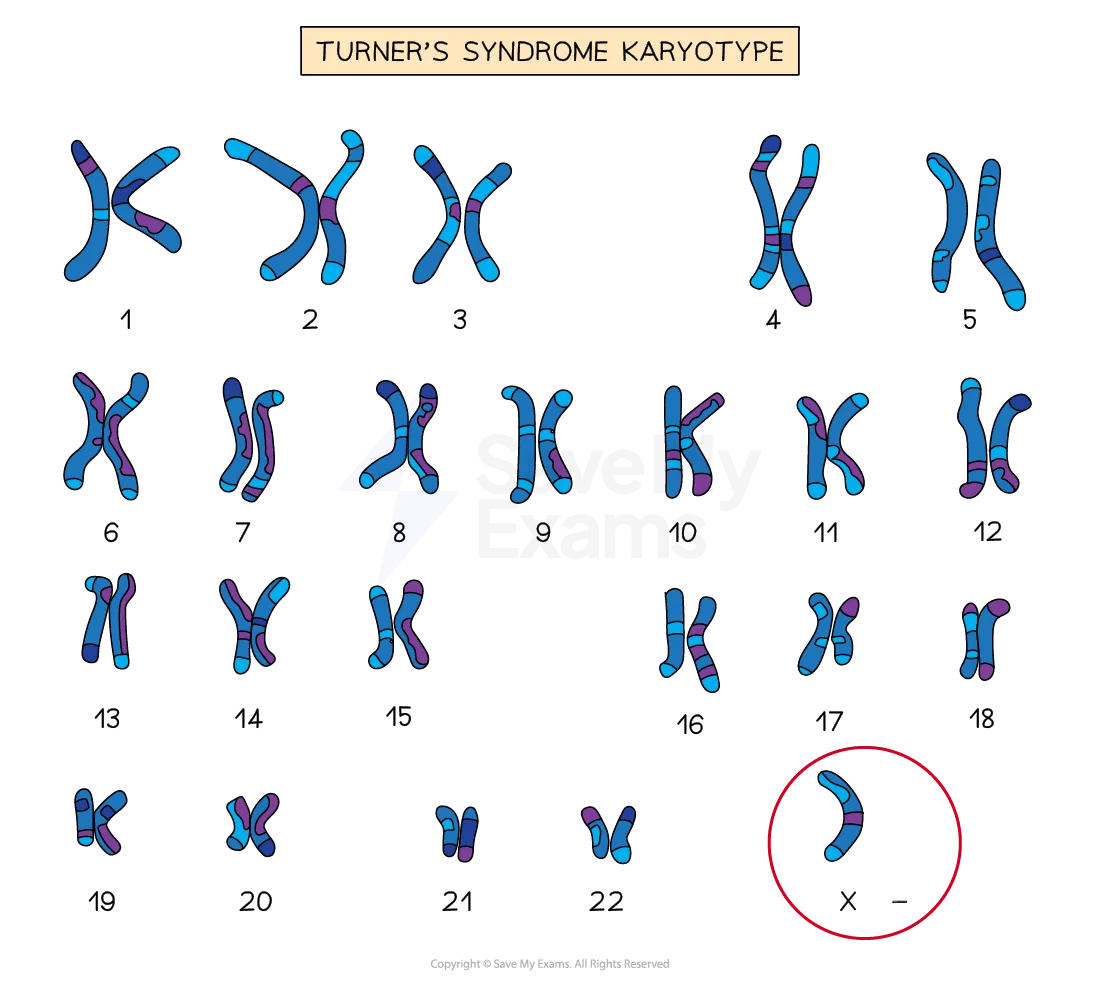
Turner's syndrome
Turner's syndrome affects about 1 in every 2,000 live female births (Turner Syndrome Support Society, 2023) and involves having all or part of an X chromosome missing, denoted by the atypical sex chromosome pattern XO
In genetic terms, the foetus is neither male nor female because the second sex-determining chromosome is absent
However, babies with TS are born and develop as females because there is no Y chromosome to direct the foetal gonads to develop male characteristics
TS occurs at conception, and the cause is not precisely known but is thought to be due to an error in the division of a parent’s reproductive cells
TS also has a ‘mosaic’ form where only some cells are affected
Most affected females will require hormone replacement therapy to develop breasts and normal female body contours, undergo proper bone growth and begin menstruation
Characteristics of Turner’s Syndrome
Physical | Cognitive |
|---|---|
Delayed onset of puberty and underdeveloped ovaries leading to menstruation problems and infertility | Usually of average or above-average cognitive ability and with a high level of verbal skill |
Short in height, with a webbed neck, narrow hips and broad shoulders | Some social adjustment problems are due to others’ responses to their appearance |
Often have heart and kidney abnormalities | Visuospatial skills may be impaired |
Research which investigates atypical sex chromosome patterns
DeLisi et al. (2005) conducted a clinical interview, cognitive tests and an MRI scan on KS and non-KS individuals and found that 10 out of 11 of the KS participants had mental health and cognitive issues and also had smaller frontal lobes, temporal lobes and superior temporal gyrus brain areas, suggesting a biological basis for their language deficits and cognitive difficulties
Quigley et al. (2014) investigated the positive effects of oestrogen replacement therapy in treating TS and found that if treated before puberty, then females with TS would have a greater increase in breast tissue, suggesting early diagnosis and treatment are vital
Evaluation of atypical sex chromosome patterns research
Strengths
Research into both KS and TS has allowed for early intervention with hormone treatment and, in some cases, the freezing of sperm or eggs to counteract the infertility of both groups
The identification of KS and TS has led to the growth of online support groups for individuals with the syndromes and their relatives, where they can be well informed about advances in knowledge and treatment, and they can communicate with others in the same position
Limitations
Research into KS and TS lacks population validity, as those who are diagnosed with these syndromes will be those with the severest symptoms and therefore research is based on an unrepresentative sample, as it excludes those who have milder symptoms, who are often those with the mosaic form
Research into both syndromes also ignores individual differences in the symptoms and progression of symptoms, meaning that diagnosis and treatment may lack validity, being based on generalised assumptions rather than on an individual basis
Issues & Debates
Diversity in sex development (DSD) conditions such as AIS, KS, and TS strongly supports the nature side of the nature vs nurture debate, as they arise from genetic and hormonal variations present from conception
However, nurture also plays a role in how individuals experience and interpret their identity and development, especially in societies with rigid gender norms
Research and treatment around DSD conditions must navigate ethical concerns, such as informed consent for early hormone treatment and the risk of medicalising natural variation
The topic is socially sensitive, especially regarding labelling, stigma, and assumptions about ‘normality’ in sex development

Unlock more, it's free!
Was this revision note helpful?
