Syllabus Edition
First teaching 2025
First exams 2027
Drug Therapy for Major Depressive Disorder (MDD) (DP IB Psychology): Revision Note
Drug therapy for MDD
Biological treatments aim to treat disorders such as MDD by targeting brain chemistry
Antidepressants are the most widely prescribed drug therapy for MDD
Types of antidepressants
Selective Serotonin Reuptake Inhibitors (SSRIs)
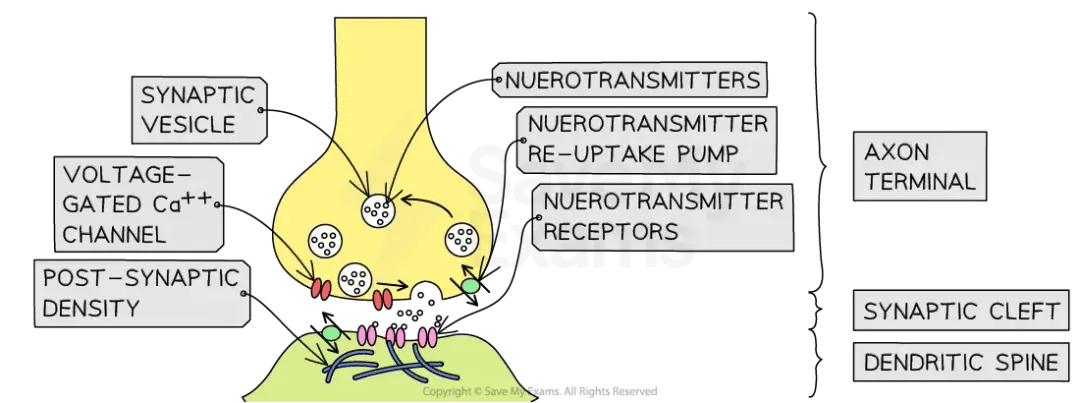
SSRIs prevent the reuptake of serotonin into the presynaptic neuron by increasing serotonin in the synaptic cleft
Examples of SSRIs that are most commonly prescribed include fluoxetine and citalopram
Serotonin-Noradrenaline Reuptake Inhibitors (SNRIs)
SNRIs work similarly to SSRIs but also increase noradrenaline
They are considered more effective for some patients
Examples of SNRIs include duloxetine and venlafaxine
Link to the monoamine hypothesis
Low or irregular serotonin levels have been linked to depressive symptoms
This supports the monoamine hypothesis, which suggests that MDD is partly due to imbalances in neurotransmitters such as serotonin
SSRIs restore balance by keeping more serotonin available in the synapse as they prevent serotonin molecules from being absorbed back into the presynaptic neuron
Research support for drug therapy & MDD
Kroenke et al. (2001)
Aim:
To compare the effectiveness of three SSRIs (paroxetine, fluoxetine, and sertraline) in treating MDD
Participants:
573 patients with MDD from 37 clinics across the USA
The participants were:
84% Caucasian, 13% Black, 3% other
79% female, 21% male aged 19–96 (mean age = 46)
Clinically recommended for SSRI treatment
Procedure:
The participants completed a baseline assessment over the telephone and were randomly assigned to one of three SSRIs (approximately 190 per group)
Treatment lasted 9 months
At 1, 3, 6 and 9 months, each participant completed:
a Mental Component Summary Score (MCSS) scale with 36 items measuring MDD symptoms
self-reports on social/work functioning, physical health, sleep, memory, and pain
Results:
79% completed the full 9-month treatment programme
Participants improved similarly across all three SSRIs (15–17 point improvement on MCSS)
Depressive symptoms decreased from:
74% at baseline
32% at 3 months
26% at 9 months
Conclusion:
SSRIs are effective in treating MDD
Paroxetine, fluoxetine, and sertraline show similar levels of effectiveness
Evaluation of drug therapy & MDD
Strengths
Reduced hospitalisation
Antidepressants have allowed many people with MDD to manage their symptoms outside hospital, giving patients more freedom and autonomy
Drug therapy is generally cheap and widely available, unlike CBT which requires trained therapists, takes longer, and often involves long waiting lists
Limitations
Although SSRIs are the most common treatment for MDD, there is a debate over their effectiveness, as some clinicians argue their effects may be little better than a placebo
There is also uncertainty about the monoamine hypothesis, as it is likely that depression is not a single disorder with one cause but a cluster of disorders with multiple underlying biological and psychological factors
Link to concepts
Responsibility
Drug therapy can be effective (see the above study) but it does not address the root cause(s) of MDD; it merely holds the symptoms at bay, with the possibility that MDD may recur later
Antidepressants may have side-effects as they work directly on the brain, so the attending clinician should monitor the patient to ensure that there are no harmful consequences of taking the drug
Change
MDD is not a stable, unchanging condition: it is subject to fluctuation and change over time
Life events, hormonal changes, illnesses for example, can determine the onset of MDD or, conversely, the reduction or elimination of the disorder from a person’s life
Drugs may be a suitable therapy for MDD at one point in someone’s life but not necessarily for every time they experience depressive symptoms
Therefore, the whole person should be considered when prescribing treatment, rather than taking the biologically reductionist route of drug therapy for every instance of MDD

Unlock more, it's free!
Did this page help you?