Tumour Development (AQA A Level Biology): Revision Note
Exam code: 7402
Tumour development
Cancer and uncontrolled cell division
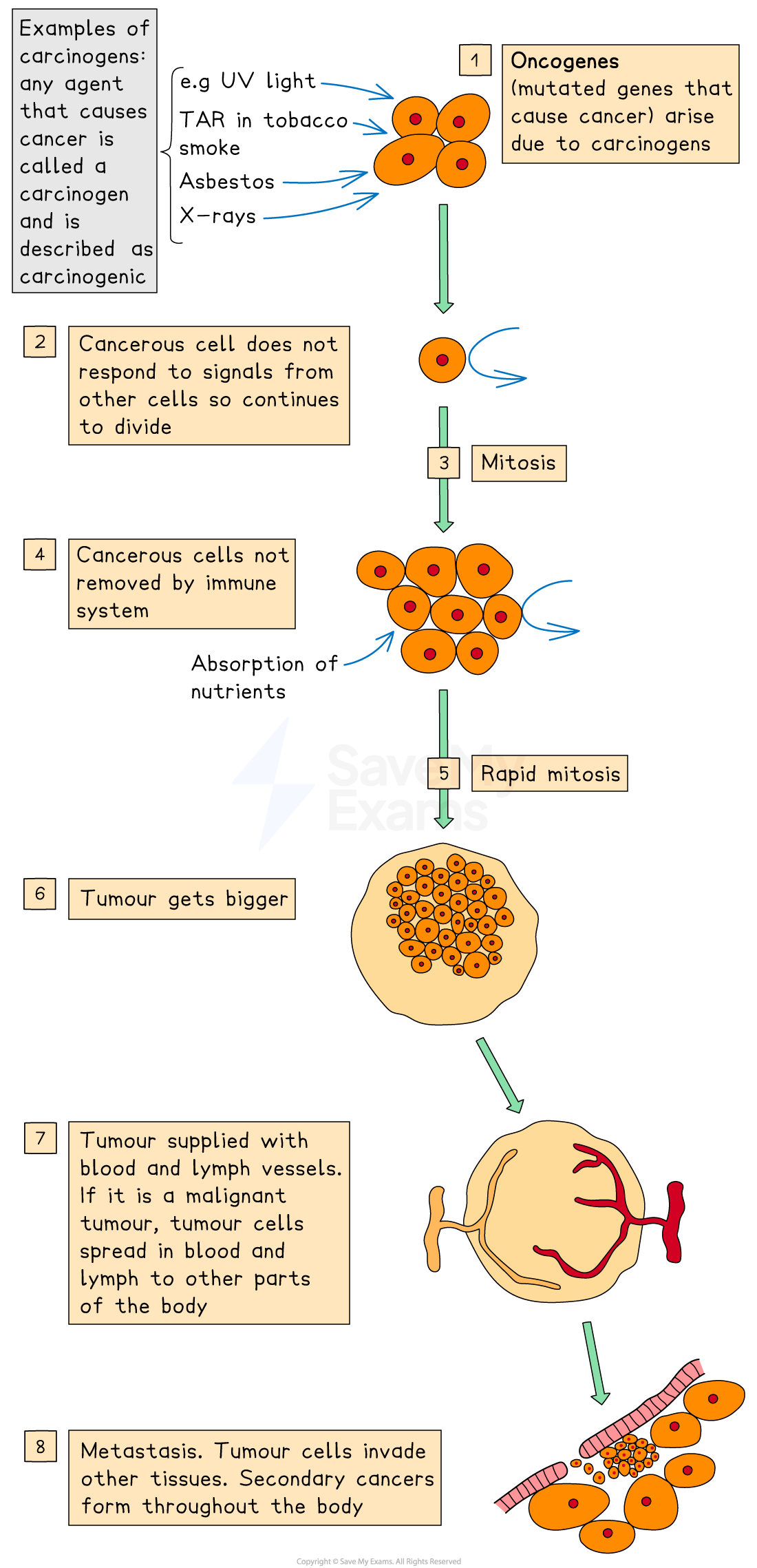
Cancer arises from uncontrolled mitosis due to mutations in genes regulating the cell cycle
Cancerous cells divide uncontrollably, forming a tumour
Mutations in genes that regulate cell division can lead to cancer; these genes may become oncogenes
Mutations are common events and don’t lead to cancer most of the time
Most mutations either result in early cell death or in the cell being destroyed by the body’s immune system
As most cells can be easily replaced, these events usually have no harmful effect on the body
Harmful mutations that escape these mechanisms can be passed to all descendant cells
Carcinogens (e.g. UV, tobacco tar, X-rays) increase mutation risk
Tumour suppressor genes
Tumour suppressor genes are normal genes which encode proteins that:
Repair DNA
Slow the cell cycle at checkpoints
Signal apoptosis if damage is irreparable
Mutations or epigenetic silencing of tumour suppressor genes can lead to tumour formation
BRCA-1 is a tumour suppressor gene mainly expressed in breast tissue
The BRCA-1 protein repairs damaged DNA or triggers apoptosis if repair fails
Reduced BRCA-1 expression leads to breast cancer development
Oncogenes
Proto-oncogenes code for proteins that stimulate cell growth and differentiation
Mutation (due to carcinogens) can convert proto-oncogenes into oncogenes
Causes constant activation of proteins that stimulate cell growth and division
This speeds up the cell cycle
If proteins that induce apoptosis are also affected, tumours can form
Oncogene activation can occur via:
inversion or translocation mutations on a proto-oncogene leading to:
increased gene expression
protein production cannot be switched off
Abnormal methylation
Abnormal methylation of DNA affects gene expression:
Increased methylation of tumour suppressor genes silences them as transcription factors are unable to bind
tumour suppressor proteins are therefore not synthesized and tumour formation occurs
RNA interference by siRNAs targeting tumour suppressor genes for breakdown can also lead to tumour development for the same reason
Reduced methylation of proto-oncogenes increases expression as the gene becomes accessible
transcription factors then bind and protein synthesis is activated
the gene behaves like an oncogene, even without a mutation
Oestrogen-dependent breast tumours
Oestrogen is a steroid hormone that upregulates transcription of certain genes through the stimulation of the ERα oestrogen receptor
High concentrations of oestrogen can lead to the development of breast cancer
High concentrations can be a result of over-expression of the oestrogen gene or from supplementary oestrogen taken in medication
~70% of breast tumours are oestrogen receptor-positive
Oestrogen enters cells, binds to oestrogen receptors in the nucleus which activates transcription
This stimulates the expression of cell cycle genes that lead to growth and replication
The drug tamoxifen is a competitive inhibitor of oestrogen:
It binds ERα receptor and prevents gene activation
This inhibits tumour growth as the oestrogen receptor cannot bind to the promoter
Examiner Tips and Tricks
In exams, you may be asked to evaluate data linking genetic and environmental factors to cancer. This often involves interpreting control group studies and understanding how risk factors lead to mutations or altered gene expression. You should apply your knowledge of oncogenes, tumour suppressor genes, and epigenetic/post-transcriptional mechanisms to explain cancer development, prevention, and treatment.

Unlock more, it's free!
Was this revision note helpful?
